Diabetes-Related Skin Conditions
Diabetes and Skin Health: Understanding the Connection
A diabetes diagnosis can often bring a variety of skin conditions and dermatological challenges. These issues can range from dry skin and persistent itching to more serious complications like infections or lesions. The link between diabetes and skin health is primarily tied to fluctuations in blood sugar levels. When blood sugar levels are elevated, the body can become dehydrated, which impairs the skin's ability to retain moisture and remain supple. This dehydration increases the likelihood of developing various skin conditions.
Proactive Care for Diabetes-Related Skin Conditions
Managing diabetes effectively is key to reducing the risk of skin-related complications. Keeping blood sugar levels within a healthy range can help prevent dehydration and maintain skin health. Additionally, regular skin checks and early intervention are essential to address any emerging skin issues before they become more serious.
If you or someone you know is dealing with a skin condition related to diabetes, don’t hesitate to schedule an appointment with a trusted expert at Cumberland Skin. Our experienced team is dedicated to supporting you on your journey to achieving and maintaining healthy skin.
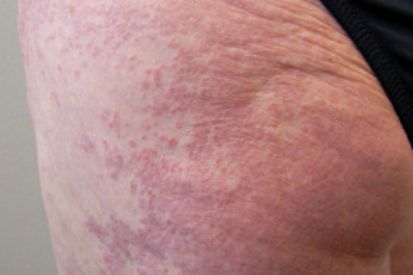
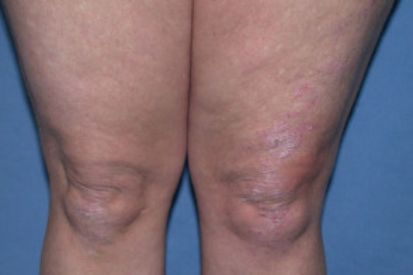
Examples of Diabetes-Related Skin Conditions



Diabetes-Related Skin Conditions Symptoms
- Acanthosis Nigricans: Dark, thick, and velvet-textured skin.
- Diabetic Blisters: On hands, toes, feet, or forearms.
- Diabetic Dermopathy: Round, brown, or purple scaly patches on shins.
- Digital Sclerosis: Thick, waxy, and tight skin on the toes, fingers, and hands.
- Disseminated Granuloma Annulare: Red or reddish-brown bull’s eye rash.
- Eruptive Xanthomatosis: Red halo that itches.
- Necrobiosis Lipoidica Diabeticorum: Large, deep spots with a shiny appearance.
- Vitiligo: White patches on the skin.
Causes of Diabetes-Related Skin Conditions
- Diabetics are more susceptible to bacterial and fungal infections; allergic reactions to medications, insect bites or foods; dry itchy skin as a result of poor blood circulation; and infections from foot injuries for people with neuropathy.
- High insulin levels
- Diabetic neuropathy
- Changes in small blood vessels
- High triglycerides
- Changes in collagen and fat underneath the skin
How to Prevent Diabetes-Related Skin Conditions
Here's a list of ways to help prevent such skin complications:
- Blood Glucose Control: Maintain target blood glucose levels through regular monitoring, medication adherence, and lifestyle modifications.
- Healthy Diet: Adopt a balanced, low-sugar diet rich in fruits, vegetables, and whole grains to regulate blood sugar levels and support overall skin health.
- Regular Skin Checks: Perform regular self-examinations to detect any changes, wounds, or abnormalities early on. Promptly address any concerns with one of our dermatologists.
- Moisturize: Keep the skin moisturized to prevent dryness and cracking. Choose fragrance-free, hypoallergenic moisturizers.
- Gentle Cleansing: Use mild, fragrance-free soaps and cleansers to avoid skin irritation. Pat the skin dry after washing instead of rubbing.
- Sun Protection: Protect the skin from harmful UV rays by using sunscreen with a high SPF, wearing protective clothing, and avoiding prolonged sun exposure.
- Regular Exercise: Engage in regular physical activity, as it can help improve blood circulation and overall skin health.
- Foot Care: Inspect and care for your feet regularly, keeping them clean and dry. Wear comfortable shoes and socks to prevent friction and pressure sores.
Diabetes-Related Skin Conditions FAQs
Diabetes impacts the skin because high blood sugar levels can lead to dehydration, making the skin dry and more prone to issues. It can also affect blood flow, making it harder for the body to heal.
Maintain stable blood sugar levels, keep your skin clean and moisturized, and be attentive to any cuts or injuries. If you notice any unusual changes in your skin, consult your dermatology provider.
Diabetes can affect the body's ability to heal. Prompt care for cuts or wounds helps prevent infections, which can be more serious for individuals with diabetes.
Choose gentle, fragrance-free products and moisturizers suitable for sensitive skin. Visit our online store for high-quality medical-grade skincare. Consult with your dermatology provider for personalized recommendations.
Contact your dermatology provider promptly. Early intervention can prevent minor issues from becoming more severe. Don't hesitate to seek professional dermatological advice for any concerns about your skin.
From Our QualDerm Family of Brands: How Diabetes Can Affect Your Skin
How to Treat Diabetes-Related Skin Conditions
Related Blog Posts

- General Dermatology
- Skin Exams
Preparing for your first dermatology appointment is important because it ensures everything goes as smoothly as possible and that your doctor is up-to-date on the status of your overall health and wellbeing. Here are our expert tips.
Read More
- General Dermatology
- Chronic Skin Conditions
Learn the differences between dry skin, eczema, and psoriasis, their distinct characteristics, and potential triggers. Gain valuable insights into identifying symptoms and seeking appropriate treatment to effectively managing these common skin conditions.
Read More
- Skin Care
- Cosmetic Treatments
Unlock the secrets to achieving radiant, glowing skin. Explore expert tips and skincare routines tailored to nourish and revitalize your complexion, empowering you to embrace a luminous and youthful appearance.
Read MoreFeatured Products

EltaMD Moisture Seal
EltaMD® Moisture Seal melts on contact and locks in moisture for up to 24 hours. It spreads easily, forming a protective layer over the skin. This intense occlusive moisturizer helps soothe dry, flaky, intact skin after procedures. This waterless, preservative-free formulation is designed for delicate skin resulting from cosmetic or medical treatments. 2.8 fl oz

Revision C+ Correcting Complex 30%
Illuminate, refine and rejuvenate skin to reveal a brilliant glow, a more even skin tone and a more youthful appearance. C+ Correcting Complex 30%™ is infused with Revision's patent-pending MelaPATH™ technology. It defends and corrects the skin-damaging effects of free radicals generated by urban dust and HEV/blue light. 1 fl oz / 30 mL


